The Evidence Speaks Series is a recurring feature highlighting the latest in Advancing Health research. This series features summaries of select publications and is designed to keep media and the research community up to date with the Centre’s current research results in the health outcomes field.
To ensure this research is quick and easy to share, you are welcome to save the social cards and use as you see fit.
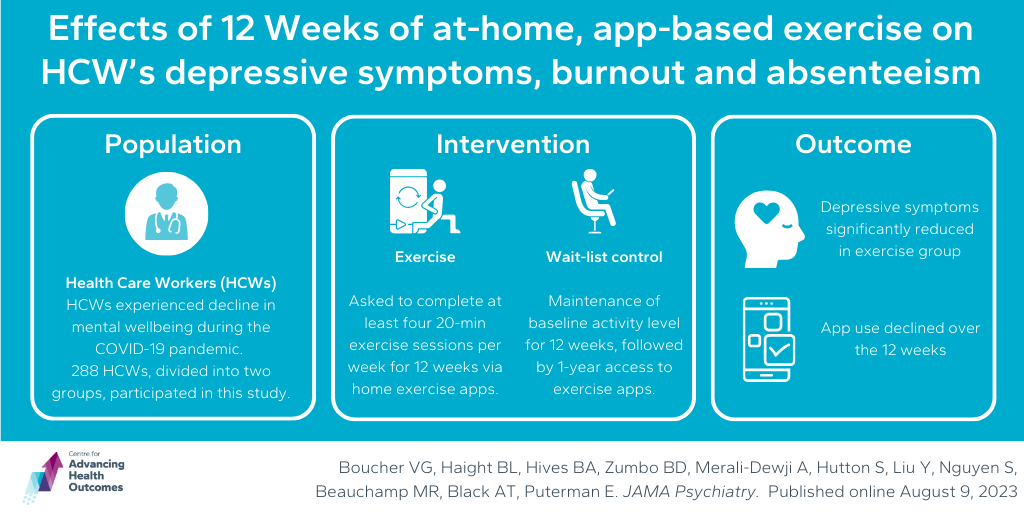
Therapeutic relationships in opioid addiction treatment can be critical to delivering personalized care
Blawatt S, Harrison S, Byres D, Foreman J, Amara S, Burdge W, MacDonald S, Schechter MT, Oviedo-Joekes E. The mobilization of nurse-client therapeutic relationships in injectable opioid agonist treatment: Autonomy, advocacy and action. J Subst Addict Treat. 2023;154:209154.
In this study, Advancing Health’s Sarin Blawatt, along with Drs. Martin Schechter and Eugenia Oviedo-Joekes, and their team, focused on the vital role of therapeutic relationships in Injectable Opioid Agonist Treatment (iOAT) for opioid use disorder. iOAT involves frequent client interactions, providing unique opportunities for healthcare engagement. This study aimed to understand how nurses in iOAT settings build therapeutic relationships and their impact on client care.
Following interviews with 24 registered nurses supporting iOAT, five key factors for fostering a culture of care in iOAT emerged: Ways of Knowing, Personal Investment, Leveraging Empathy, Finding Flexibility, and Collaborating to Overcome. These factors help create a safe, nonjudgmental environment where nurses build trust and identify client needs beyond medication administration. Nurses also engage in team-based problem-solving to advocate for clients.
This research underscores the importance of therapeutic relationships in delivering personalized care and bridging client needs and program access. Expanding access to iOAT programs and their embedded services is crucial for better serving individuals with diverse needs in the context of opioid addiction treatment.
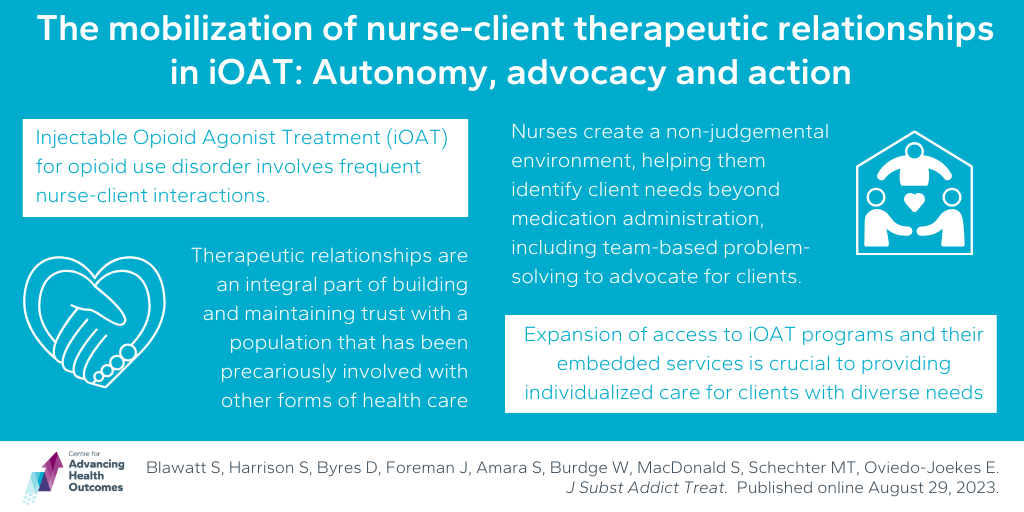
Lowering colorectal cancer screening age
Kalyta A, Ruan Y, Telford JJ, De Vera MA, Peacock S, Brown C, Donnellan F, Gill S, Brenner DR, Loree JM. Association of reducing the recommended colorectal cancer screening age with cancer incidence, mortality, and costs in Canada using OncoSim. JAMA Oncol. Published online July 20, 2023.
Colorectal Cancer (CRC) screening in Canada typically begins at age 50. A team including Advancing Health Scientists Drs. Mary De Vera and Carl Brown used computer modelling via the OncoSim platform to simulate different scenarios to explore the potential benefits of starting CRC screening sooner.
Starting screening at age 45 led to 12,188 fewer CRC cases, 5,261 fewer CRC-related deaths, and an additional 92,112 quality-adjusted life-years (QALYs) over a 40-year period compared to starting at age 50. If screening began at age 40, there were even greater benefits, with 18,135 fewer CRC cases, 7,988 fewer deaths, and 150,373 QALYs gained.
Despite increased upfront costs of earlier screening and treatment, the overall healthcare system cost for managing CRC decreased. This suggests that initiating screening at a younger age could be a cost-effective way to reduce the burden of CRC in Canada. However, further evaluation of the impact on colonoscopy capacity is needed before implementing any changes to screening guidelines.
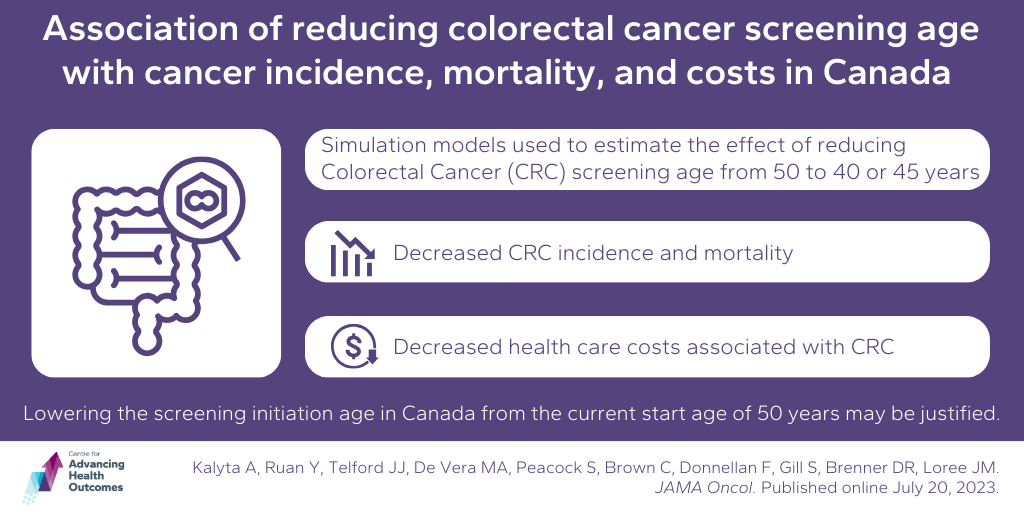
12-week exercise program improves health care workers’ wellbeing
Boucher VG, Haight BL, Hives BA, Zumbo BD, Merali-Dewji A, Hutton S, Liu Y, Nguyen S, Beauchamp MR, Black AT, Puterman E. Effects of 12 weeks of at-home, application-based exercise on health care workers’ depressive symptoms, burnout, and absenteeism. JAMA Psychiatry. 2023;80(11).
During the COVID-19 pandemic, healthcare workers (HCWs) experienced a decline in their mental well-being. Advancing Health’s Agnes Black and team conducted a study to explore whether a 12-week exercise program could alleviate depressive symptoms among HCWs. They recruited 288 HCWs from a B.C. urban healthcare organization, randomly assigning half to a waitlisted control group and half to an exercise group who were given access to variety of home exercise apps (yoga, cardio, strength training). They were asked to engage in four 20-minute sessions per week over 12 weeks.
Researchers assessed depressive symptoms, burnout levels, and sick days every two weeks. Results showed a significant drop in depressive symptoms for the exercise group, as well as fewer sick days, and cynicism and emotional exhaustion (two facets of burnout) improved. However, app usage dwindled over time, with only 23% maintaining regular use.
These results demonstrate exercise’s potential for improving HCW’s mental health while also highlighting the challenge of sustaining motivation for exercise and the necessity of strategies to encourage HCWs to maintain their exercise routines for ongoing mental health benefits.