The Evidence Speaks Series is a recurring feature highlighting the latest in Advancing Health research. This series features summaries of select publications and is designed to keep media and the research community up to date with the Centre’s current research results in the health outcomes field.
To ensure this research is quick and easy to share, you are welcome to save the social cards and use as you see fit.
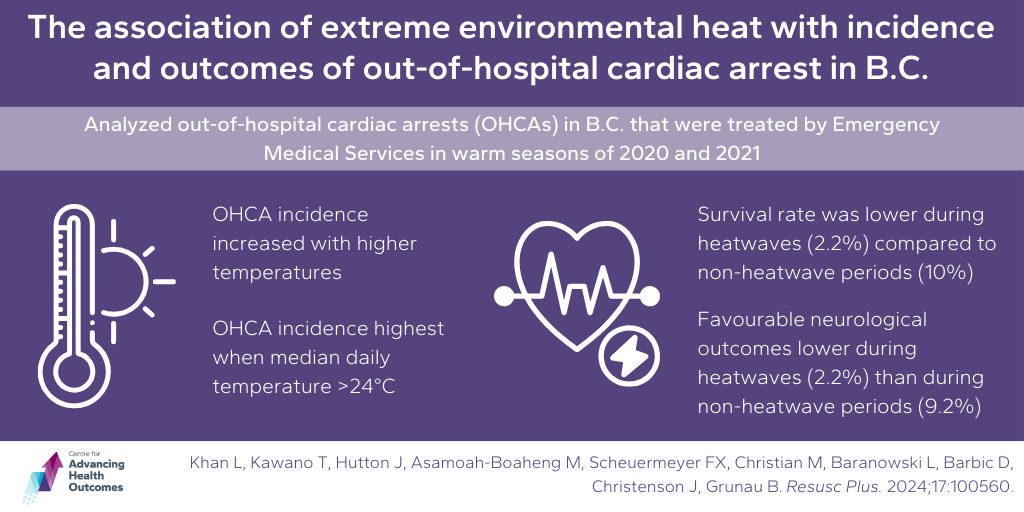
Heatwaves may increase cardiac arrests and decrease survival
Khan L, Kawano T, Hutton J, Asamoah-Boaheng M, Scheuermeyer FX, Christian M, Baranowski L, Barbic D, Christenson J, Grunau B. The association of extreme environmental heat with incidence and outcomes of out-of-hospital cardiac arrest in British Columbia: A time series analysis. Resusc Plus. 2024 Mar;17:100560.
With average temperatures rising, extreme heat events are expected to occur with increased frequency and intensity in the future. As extreme heat is associated with increased mortality, Advancing Health Scientists Drs. Frank Scheuermeyer, Jim Christenson, and Brian Grunau, PhD trainee Jacob Hutton, and postdoctoral fellow Dr. Michael Asamoah-Boaheng sought to understand how extreme heat affects out-of-hospital cardiac arrests (OHCA) in B.C. The team looked at OHCAs in B.C. that were treated by Emergency Medical Services (EMS) during the warm seasons of both 2020 and 2021. They found that as temperatures rose, the incidence of OHCA increased significantly, especially during heatwaves. Among people treated by EMS for OHCA, survival rates during heatwaves were lower compared to non-heatwave periods, with only 2.2% surviving and having favourable neurological outcomes, compared to 10.0% and 9.2% during non-heatwave periods. This suggests that extreme heat poses a significant risk for OHCA and negatively impacts patient outcomes. While the study focused on B.C., similar patterns have been observed in other regions globally. Understanding these effects is crucial for emergency services to prepare for and mitigate the impacts of heatwaves on public health.
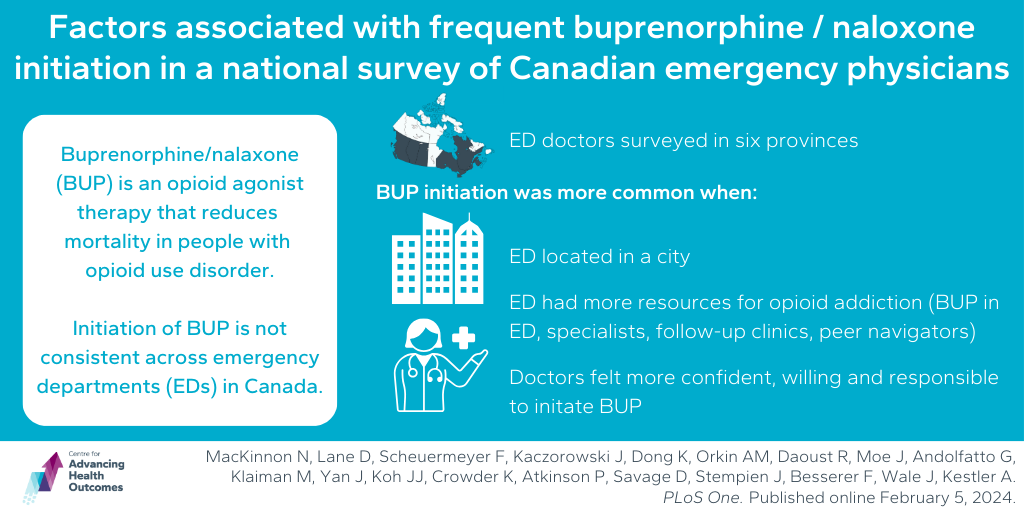
Increased training and resources may increase initiation of treatment for opioid use disorder in emergency departments
MacKinnon N, Lane D, Scheuermeyer F, Kaczorowski J, Dong K, Orkin AM, Daoust R, Moe J, Andolfatto G, Klaiman M, Yan J, Koh JJ, Crowder K, Atkinson P, Savage D, Stempien J, Besserer F, Wale J, Kestler A. Factors associated with frequent buprenorphine / naloxone initiation in a national survey of Canadian emergency physicians. PLoS One. Published online February 5, 2024.
Initiation and maintenance of opioid agonist therapy (OAT) is an evidence-based strategy that reduces mortality for people with opioid use disorder (OUD). Given that people with OUD have a high attendance in emergency departments (EDs), EDs are an opportune setting to initiate first-line OAT, buprenorphine/naloxone (BUP). However, BUP initiation varies widely across Canadian EDs. Advancing Health’s Drs. Frank Scheuermeyer and Andrew Kestler aimed to understand why some emergency departments (EDs) in Canada frequently start patients BUP for opioid addiction, while others do not. They surveyed emergency doctors in six different provinces and analyzed factors including the doctors’ attitudes and the resources available at their ED. They found that certain factors, like having more resources for opioid addiction treatment and being located in a city, were linked to more frequent BUP initiation. Also, doctors’ attitudes, like feeling confident and responsible to start BUP, played a role. Providing better training for doctors and increasing resources for treating opioid addiction in EDs could help more patients receive BUP.
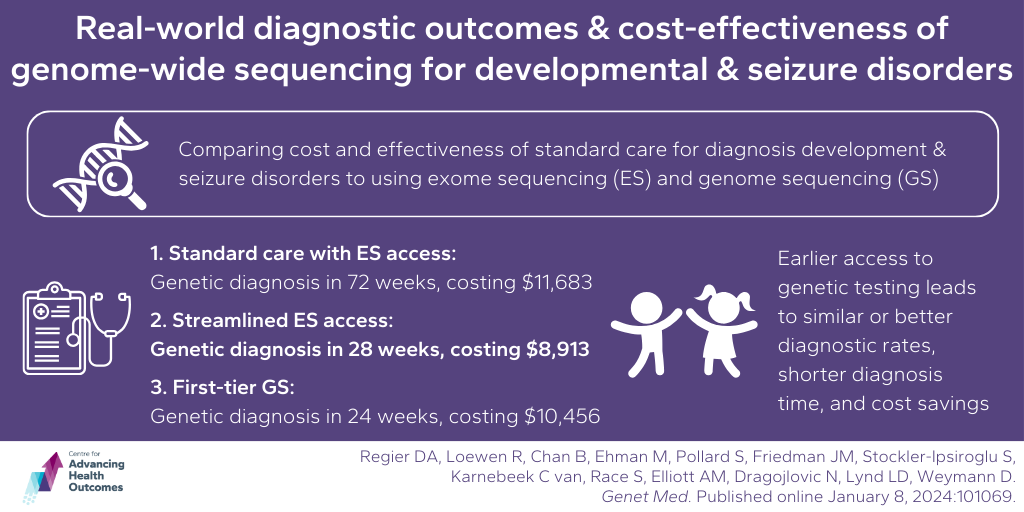
Earlier access to genetic testing may lead to quicker diagnoses for childhood developmental and seizure disorders and save money in the Canadian health care system
Regier DA, Loewen R, Chan B, Ehman M, Pollard S, Friedman JM, Stockler-Ipsiroglu S, Karnebeek C van, Race S, Elliott AM, Dragojlovic N, Lynd LD, Weymann D. Real-world diagnostic outcomes and cost-effectiveness of genome-wide sequencing for developmental and seizure disorders: evidence from Canada. Genet Med. Published online January 8, 2024:101069.
Advancing Health’s Dr. Larry Lynd co-authored a study aimed at understanding the effectiveness and cost of using exome sequencing (ES) and genome sequencing (GS) for diagnosing developmental and seizure disorders in children in B.C. The team analyzed data from 491 patients who underwent standard diagnostic testing at B.C. Children’s Hospital and compared it to three diagnostic strategies: standard care with limited ES access (as a last resort following chromosome test, biochemical and single-gene testing), streamlined ES access (ES received if no diagnosis from chromosome test), and first-tier GS (patients immediately receive GS, which is a more all-encompassing genetic test than ES). The results indicated that earlier access to ES or GS led to similar or better diagnostic rates and shorter diagnosis times compared to standard care. Streamlined ES and first-tier GS were also found to potentially save costs, with streamlined ES offering the most significant cost savings. For standard care, the expected cost per patient was $11,683 over 10 years with an estimated time to genetic diagnosis of 72 weeks. Streamlined access to ES resulted in a time to diagnosis of 28 weeks, with a 10-year mean cost of $8,913, and for the first-tier GS strategy, the expected cost was $10,456 with a time to genetic diagnosis of 24 weeks. This suggests that providing earlier access to genetic testing could lead to quicker diagnoses and cost savings in the Canadian health care system. A quicker diagnosis is valuable to patients, their families, and health care systems by reducing health care interactions, mis-diagnoses, and unnecessary clinical interventions.